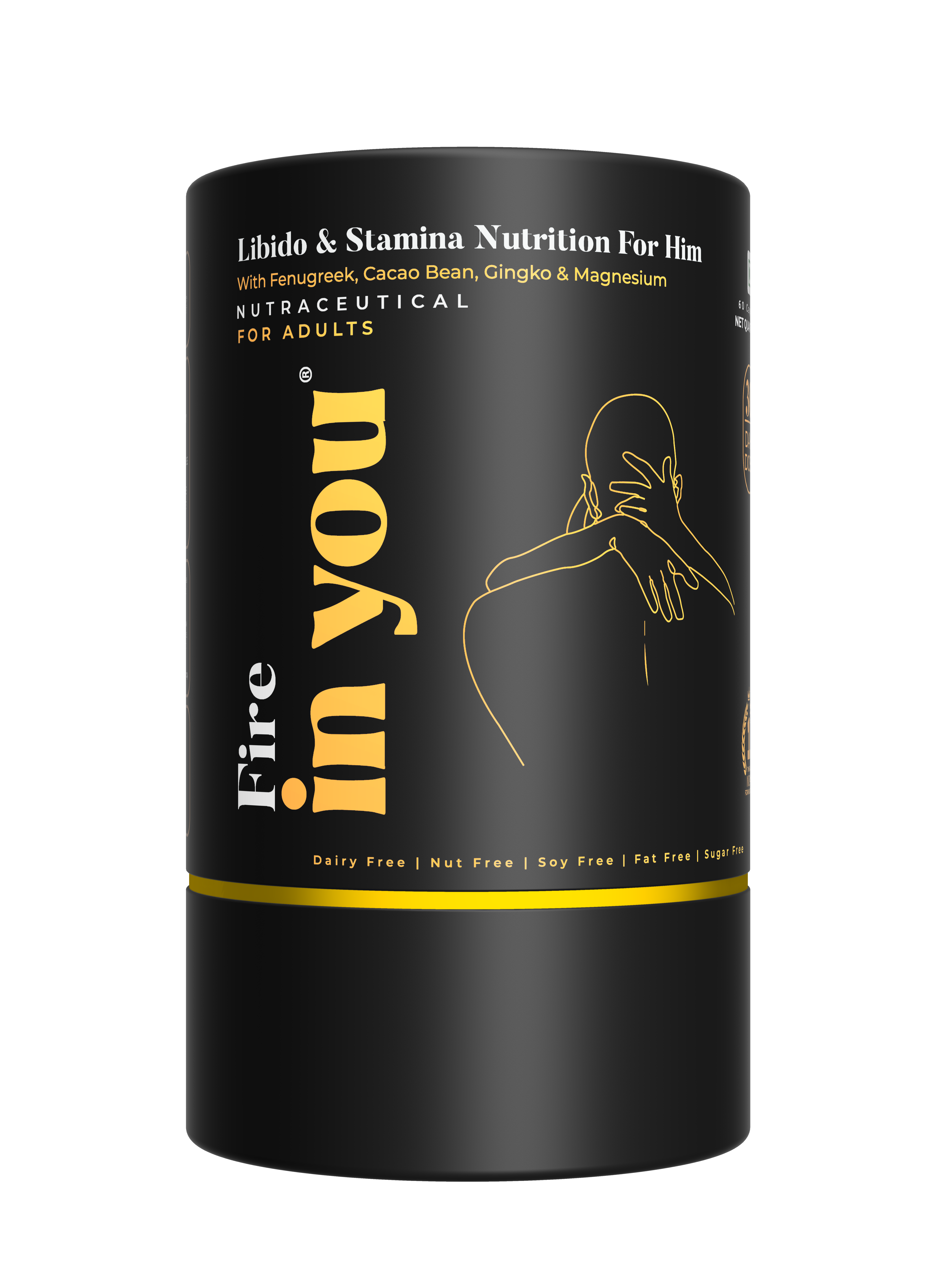
- products
- Science
- wellness journal
- About Us
- Faqs
- Sustainability
- Contact Us
- Self Test
- English

Did you know that over 50% of individuals diagnosed with depression report a noticeable decrease in their sex drive? In the year 2022, this fascinating statistic was published in “Nature”. The connection that this statistic establishes between mental health and sexual desire is something that I have observed in my practice as well. To truly understand sex drive, we also have to consider the holistic impact of stress, anxiety, and depression on their sexual health.
What is Sex Drive?
Sex drive, also known as libido, refers to the overall desire for sexual activity, whether having sex with a partner or through masturbation. Several factors can influence it, including biological elements like hormones (testosterone, oxytocin) and neurotransmitters (dopamine, noradrenaline), along with psychosocial factors such as age, gender, living conditions, stress, and anxiety.
Libido naturally differs greatly from one individual to another, depending on factors like age, life situations, and personal preferences. There is no universally accepted “normal” level of libido or a “correct” frequency for sexual activity.
Low libido is a common problem presenting in sexual health clinics, with a prevalence ranging from 20-30% of the population. Women, particularly those in the post-menopausal stage of life, have a higher incidence of this condition than men of senior age groups. Several factors can contribute to low libidos, such as relationship issues, medical conditions, mental health problems, certain medications, and ageing.
“Understanding libido is crucial as various factors, including stress, anxiety, and depression, can significantly alter it.”
In this blog, you are going to explore the impact of stress, anxiety, and depression on libido, the underlying biological mechanisms, and practical strategies to manage these effects.
Understanding the Impact of Stress on Sex Drive
Consider the case study of a 35-year-old woman under immense work pressure. Over time, she noticed herself losing interest in her hobbies, in spending time with her husband and also in any sexual activity at all. The couple consulted a healthcare professional, wondering if there was a hormonal reason for the change. The panel only showed an elevation in cortisol and a decline in testosterone levels, and that’s how she learnt that it was her stress levels causing her decreased libido.
Stress is the body’s response to perceived threats, triggering the nervous system and activating coping mechanisms. While short-term stress is manageable and doesn’t leave an impact on the body, prolonged stress can lead to significant health issues. Most of these are a direct or indirect effect of the stress hormone “cortisol”.
Every little stress induces the body to release cortisol, which enables it to cope with the fight or flight response. In cases of chronic stress, cortisol remains persistently elevated. This may result in a decrease in testosterone levels, a hormone vital for sexual desire in both men and women. As a result, this hormonal imbalance may cause a lowered libido or sex drive, causing a decreased interest in sexual activities.
The Role of Anxiety in Sexual Health
A ubiquitous presentation in my clinic is patients who walk in, anxious about their performance during intimate moments. This performance anxiety creates a vicious cycle, where their fear of not performing well leads to sexual dysfunction during critical moments, which results in further anxiety, eventually resulting in a complete loss of interest in any sexual activity.
Anxiety can manifest in various forms, all of which exacerbate feelings of inadequacy. Anxiety also triggers physiological responses, such as increased heart rate and muscle tension, which can hinder sexual arousal and performance. For instance, men may experience erectile dysfunction or delayed ejaculation due to anxiety, while women may struggle with lubrication or orgasm. Such performance issues can cause sex to become an unsatisfactory or, sometimes, unpleasant experience for the person, and naturally, the brain starts rejecting such occurrences, leading to a lack of sexual desire and decreased sex drive.
Depression and Its Effects on Libido
Depression is a medical condition marked by prolonged feelings of sadness, a loss of interest in previously enjoyable activities (including sex), and a persistent lack of energy. Many of these symptoms are due to neurotransmitter imbalances in the brain, including serotonin, dopamine, and noradrenaline.
These very neurotransmitters also regulate sex drive. Change in sex drive is a crucial diagnostic symptom for depression, which mental health practitioners look at. Fatigue, negative self-perception, and relationship strain can also diminish sexual interest.
A key point to remember is any mental health issue, such as depression and anxiety, triggers a stress response in the body. Along with the neurotransmitter inefficacy, there are elevated levels of cortisol circulating in the body for the duration of the mental illness, which further contributes to sexual dysfunction.
Tips for Managing Stress, Anxiety, and Depression
1. Prioritize self-care: Participate in activities that encourage relaxation and overall well-being, such as exercise, yoga, meditation, or pursuing hobbies.
2. Open communication: Open dialogue within the relationship about each others’ needs and concerns can strengthen intimacy, reduce performance anxiety and help overcome many barriers to a healthy sex life.
3. Maintain a balanced lifestyle: A healthy diet, regular exercise, 6-8 hours of sleep, and work-life balance. All of these, play a major role in recovery from stress and depression.
4. Educate Yourself: Education about sex, sexual behaviours, and sexual responses may help overcome anxieties about sexual function.
5. Seek professional help: Consult with a mental health professional to address underlying issues and explore treatment options, including lifestyle modifications, therapy, and medication. Explore the role of couple therapy in addressing sexual dysfunction related to mental health issues.
Common Myths and Misconceptions
Myth: Men should always be interested in sex.
Fact: Multiple biopsychosocial factors affect male libido- such as age, life circumstances, stress levels and health conditions. While low desire conditions are more commonly seen in women, men are also equally susceptible and can benefit from lifestyle modifications, therapy and medication.
Myth: (A fixed weekly frequency indicates normal libido)
Fact: Libido is a subjective feature and varies widely from person to person. There are no “normal” levels of libido, nor can it be measured by the frequency of sexual practices.
Conclusion
In summary, stress, anxiety, and depression can significantly impact sexual desire, creating a complex interplay that affects both mental and sexual health. Understanding these connections is vital for individuals seeking to improve their quality of life. If you or someone you know is struggling with these issues, consider consulting a healthcare professional for support and guidance. Proactively improving mental well-being can lead to healthier relationships and a more fulfilling sex life. Keep in mind that sexual health is a vital component of overall wellness.
Author:

Dr. Ooha
Reviewed By:
Dr. Indraneel
Source:

Dr. Ooha
Dr. B Ooha Sumita graduated with MBBS from the prestigious Armed Forces Medical College (AFMC) and obtained her MD in Psychiatry from NTR University of Health Sciences. She has over 9 years of clinical experience and now practices as a neuropsychiatrist. She has experience in dealing with varied mental health issues such as depression and anxiety, schizophrenia, OCD, bipolar disorder, ADHD and autism, and addictions. She has also completed specialized courses in reproductive mental health and sexual medicine. Dr. Ooha is an intuitive practitioner and prefers a patient-centric approach to treatment. Her patients usually recommend her for patient listening and clear explanations.


Embrace your body, ignite intimacy, and unlock boundless pleasure.
Related Products
Get 10% off
on your first order
You’ll also get dibs and a heads up on any sales or product launches.