- products
- Science
- wellness journal
- About Us
- Faqs
- Sustainability
- Contact Us
- Self Test
- English

Imagine a sling or hammock holding your entire weight and keeping you away from the ground while you peacefully relax and function. Your pelvic floor muscles are like that trusty hammock, holding everything from your bladder, bowels, uterus or the prostate. Weakening of this trusty ‘hammock’ a vital part of the body, can lead to pelvic floor dysfunctions.
The pelvic floor consists of several muscles creating a dome-shaped diaphragm stretching from the pubis to the hip bone. It supports the pelvic organs, helps in the continence of bodily excretion and promotes the sexual functions of orgasm.
Pelvic floor dysfunctions can affect both men and women leading to a series of issues such as incontinence and sexual dysfunctions. This blog will cover how targeted rehabilitation can restore the strength and function of these vital muscles.
Understanding Pelvic Floor Dysfunctions
The pelvic floor muscles are the base foundation for your organs and help in supporting the vital body organs. The simple action of going to the bathroom occurs because the pelvic floor muscles tighten and relax, helping in emptying bodily waste such as urine. Dysfunction in these muscles can result in constant tightening instead of relaxing and hence cause increased tension. This can lead to an incomplete bowel movement, pain during intercourse or a problem in maintaining an erection.
Some symptoms of pelvic floor dysfunction can be; frequently using the bathroom, straining to pass a bowel movement, constipation, and painful urination. Along with this women with PFD report decreased arousal and infrequent orgasms. According to reports 65.8% of women above the age of 40 complain of PFD and sexual dysfunction. The pelvic muscles can weaken due to various reasons such as ageing, pelvic surgery, childbirth, traumatic injury or obesity (1).
Training and strengthening your pelvic floor muscles are considered a powerful and non-invasive method of rehabilitation. Pelvic physiotherapy has exponential potential in treating such disorders among men and women.
Pelvic Floor Rehabilitation: How to get started?
When it comes to pelvic floor rehabilitation, the approach is both scientific and personalized. Understanding the precise nature of the pelvic floor muscles and their role in overall pelvic health is crucial to developing effective treatment plans.
40 men suffering from lifelong premature ejaculation were treated with a 12-week pelvic floor muscle rehabilitation regimen (2). The results shown were promising and presented a low-cost effective treatment than the standard. Pelvic floor muscle rehabilitation is a viable therapeutic option for treating sexual dysfunction in men and women.
It is important to not self-diagnose this condition and visit a medical professional who can identify the root cause and render a customised treatment plan. Pelvic floor rehabilitation can include a range of physical therapy techniques to strengthen and relax those muscles.
Identifying your pelvic muscles
The foremost step of doing so includes identifying the right muscle. The next time you start urinating, stop and feel the muscles that are contracting to stop the flow. The muscles that you’ll feel tighten and love up and the pelvic floor muscles. You need to utilise these muscles to perform pelvic exercises. However, once you can comfortably identify your muscles, make sure that you perform this exercise when seated and NOT during urination.
Weighted vaginal cones are another method for women to help them in controlling their pelvic muscles. A weighted vaginal cone is inserted in the vagina and women are asked to practice holding it in by using pelvic muscle contractions. This provides the brain with active sensory feedback and increases efficacy over no active treatments.
Men can identify this muscle by inserting a finger in the rectum and trying to squeeze it. Another way includes tensing the muscles that prevent the passing of gas (3).
Performing Pelvic Floor Exercises
Kegel exercises can improve sexual function and improve the strength of the pelvic floor muscles. These are simple exercises that can be done anytime and anywhere.
Start practising kegel exercises on an empty bladder. To start, tense your pelvic muscles and maintain that tension to a count of five. Relax and release the muscles to the same count. Over the next few days, start training your muscles to stay tense to a count of 10 and repeat the exercise three times every day.
If you feel pain after doing kegel exercises, it might be a sign that you aren’t engaging the right muscles. In such cases, it is essential to talk to a health professional and practice exercises with a therapist. It is important to not overdo these exercises as they can cause muscle fatigue and increase incontinence (4).
Biofeedback
This technique uses sensors to provide real-time feedback on muscle activity. It helps patients learn how to properly engage and control their pelvic floor muscles. A therapist inserts a sensor into the vagina or rectum to measure muscle contractions, providing valuable insights into muscle performance and aiding in effective training.
This technique is also used as a positive reinforcement method. A therapist can motivate and asses the learning progress of the patient (5).
Electrical Stimulation
Low-level electrical currents are used to stimulate the pelvic floor muscles. This can be particularly helpful for patients who have difficulty engaging these muscles on their own. Electrical stimulation enhances muscle contraction and helps in re-educating the muscles
Electrical stimulation facilitates the contraction of the pelvic muscle passively. This enables the patient to become aware of the muscles and improve the tonality and strength of the contraction (5).
Lifestyle modifications
Avoiding alcohol, caffeine, concentrated sugar, acidic food and beverages are some dietary modifications that can improve anorectal symptoms. It would also be beneficial to restrict spicy foods, artificial sweeteners and cigarettes to improve symptoms of incontinence.
Adopting a healthy lifestyle along with exercise can also help with weight loss. Obesity stresses the pelvic floor and can also affect the functioning of the nerves and muscles of the genital tract. Reports suggest that a 3% to 5% reduction in weight can decrease episodes of urinary incontinence (6).
Good bathroom habits
Social media and Instagram have led to an increase in the time spent on the pot. This can harm the pelvic floor muscles and eventually decrease control over your bladder and bowels. It’s important to develop good bathroom habits like getting up and getting out once your business is done.
Holding in urine for a long period can strain your muscles and weaken them; go to the bathroom whenever you feel the urge to urinate. Avoid straining your muscles during passing stools. If you have difficulty in emptying your rectum, eat fibrous food and drink plenty of water to ensure easy bowel movement.
Conclusion
Pelvic muscles are a vital part of our body, however, they are often overlooked. Pelvic floor dysfunction can cause various issues in men and women likewise. It can range from decreased sensation with sexual activity, delayed arousal, pain during intercourse, urinary incontinence, pelvic organ prolapse etc.
The prime objective of pelvic floor rehabilitation includes providing patient-centred care. Physicians and therapists work in tandem to deliver effective and empathetic care. The treatment can range from medications and patient education to physical therapy. Pelvic floor exercises are a behavioural treatment for improving and strengthening the function of the pelvic muscles. These exercises may take time to master but can work as an effective treatment regimen.
Author:

Dr Tanya Prasad
Orthodontist
|BDS, MCODS (Manipal) MDS - SDS, KVV (Karad)
Reviewed By:
Dr. Indraneel
Medical Writer
Source:
1. Li-Yun-Fong RJ, Larouche M, Hyakutake M, Koenig N, Lovatt C, Geoffrion R, Brotto LA, Lee T, Cundiff GW. Is Pelvic Floor Dysfunction an Independent Threat to Sexual Function? A Cross-Sectional Study in Women With Pelvic Floor Dysfunction. J Sex Med. 2017 Feb;14(2):226-237. doi: 10.1016/j.jsxm.2016.11.323. Epub 2016 Dec 29.
2. Pastore AL, Palleschi G, Fuschi A, Maggioni C, Rago R, Zucchi A, Costantini E, Carbone A. Pelvic floor muscle rehabilitation for patients with lifelong premature ejaculation: a novel therapeutic approach. Ther Adv Urol. 2014 Jun;6(3):83-8. doi: 10.1177/1756287214523329.
3. Cho ST, Kim KH. Pelvic floor muscle exercise and training for coping with urinary incontinence. J Exerc Rehabil. 2021 Dec 27;17(6):379-387. doi: 10.12965/jer.2142666.333.
4. Pelvic floor muscle training exercises: MedlinePlus Medical Encyclopedia [Internet]. Medlineplus.gov. 2017. Available from: https://medlineplus.gov/ency/article/003975.htm
5. García-Perdomo HA, Rodes MC. From Kegel exercises to pelvic floor rehabilitation: A physiotherapeutic perspective. Revista Mexicana de Urología. 2018 Oct 19;78(5).
6. Subak LL, Wing R, West DS, Franklin F, Vittinghoff E, Creasman JM, et al. Weight Loss to Treat Urinary Incontinence in Overweight and Obese Women. New England Journal of Medicine. 2009 Jan 29;360(5):481–90.

Dr Tanya Prasad
Orthodontist
|BDS, MCODS (Manipal) MDS - SDS, KVV (Karad)
Dr Tanya Prasad is an Orthodontist and a medical health writer with a work experience of 4+ years. She has several Patents, Copyrights and scientific publications credited to her name. Along with being a literature enthusiast she enjoys reading fiction in her free time.


Embrace your body, ignite intimacy, and unlock boundless pleasure.
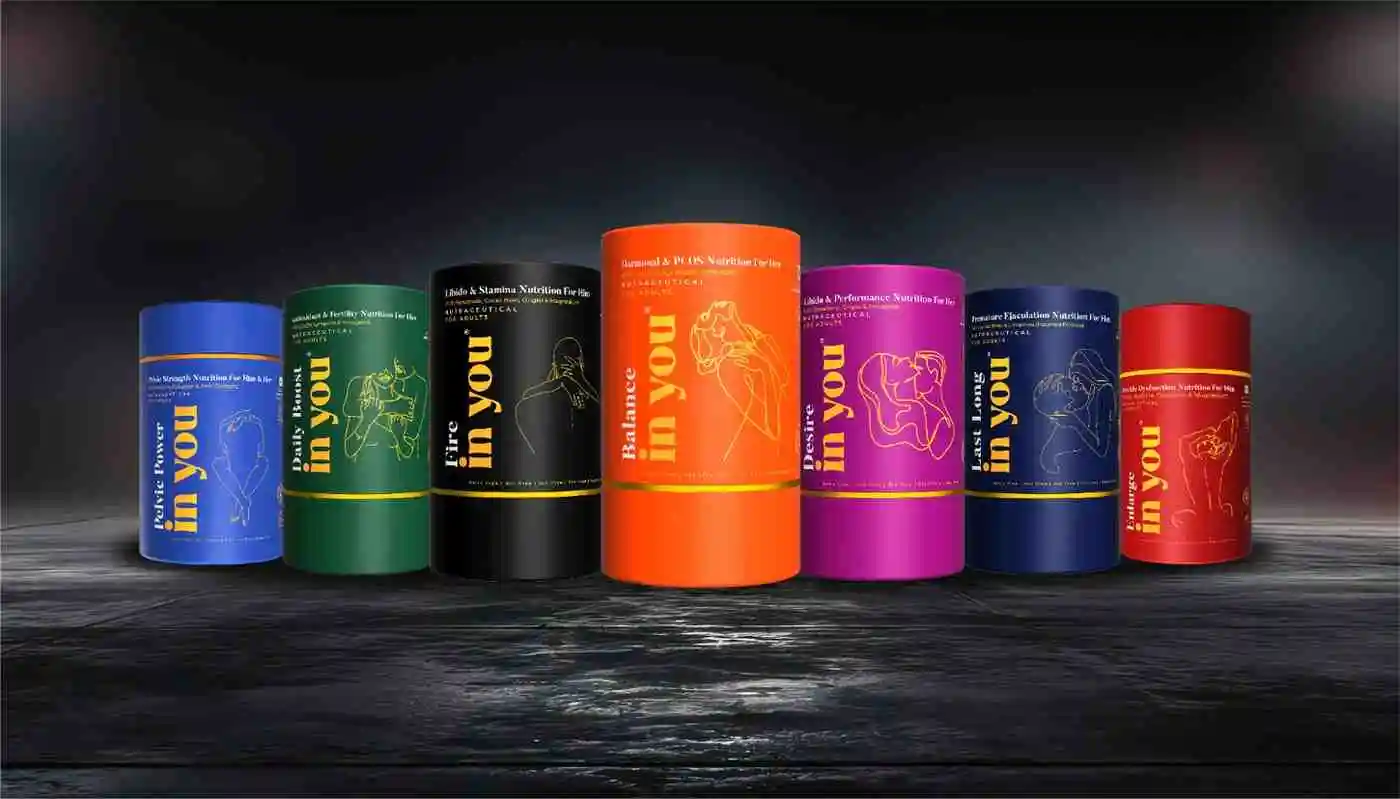
Related Products
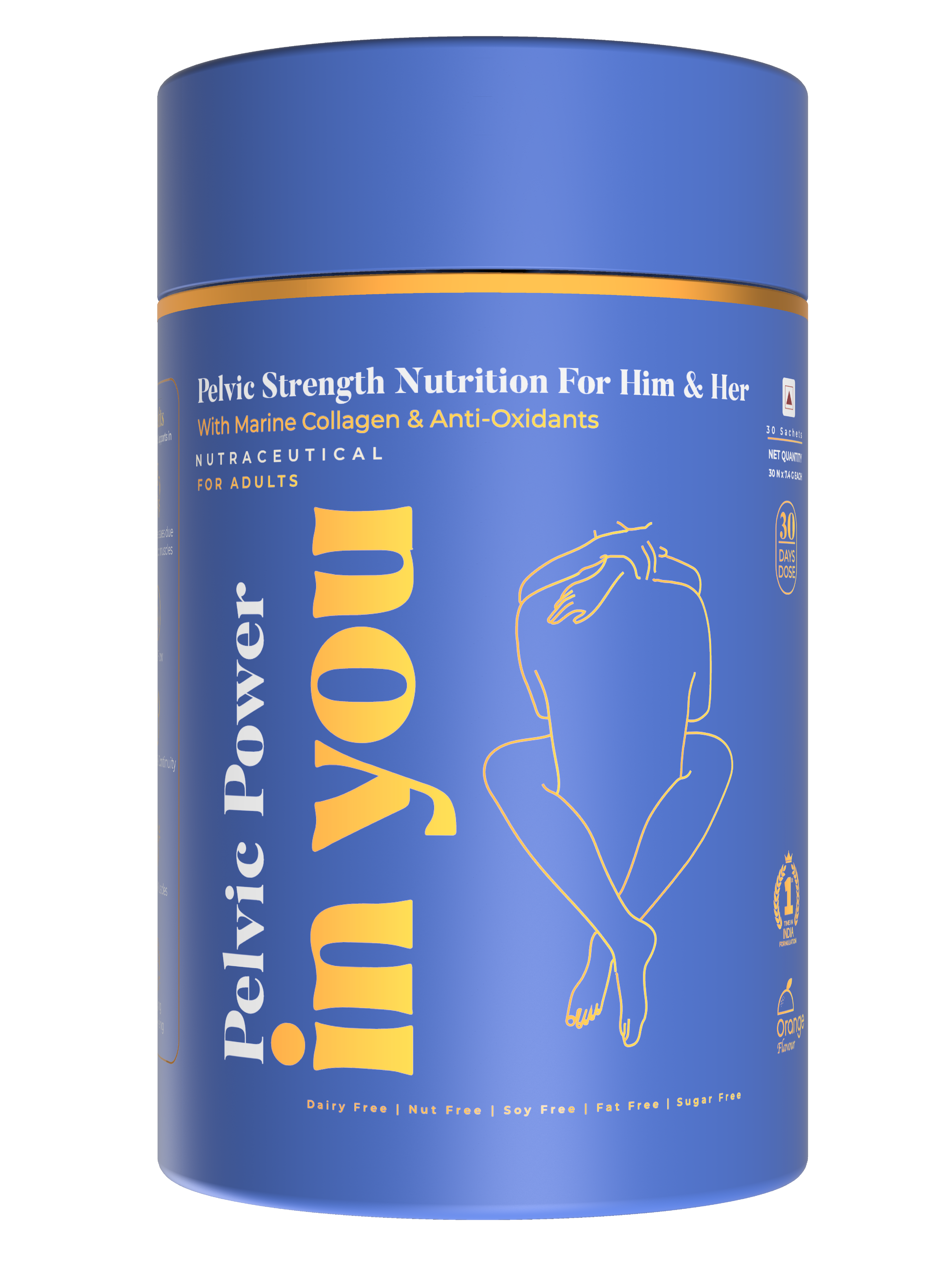
InYou Pelvic Power Collagen & Antioxidant Blend for Core Strength supplement for Both Him and Her - 30 Sachets
₹2199
Buy NowGet 10% off
on your first order
You’ll also get dibs and a heads up on any sales or product launches.